Arthritis and Joint Disorders: Symptoms and Treatment
Arthritis is one of the most prevalent chronic health conditions, constituting a significant source of pain and disability around the globe. While some people associate the condition solely with ageing, arthritis can affect people of any age, including children. Furthermore, arthritis is not a single disease; rather, it is a collective term for more than 100 disorders that affect the joints and surrounding tissues.
Arthritis can range from mild discomfort to significant joint damage, restricting a person’s ability to move and perform daily activities. Learning the different forms of arthritis, their causes, and their treatment options will enable individuals to identify symptoms earlier and take measures to protect their joints.

What is Arthritis and Joint disorders?
Arthritis is defined as the inflammation of one or more joints. A joint is the area in which two bones come together to create a fulcrum for movement and a stable support. Healthy joints have a cushioning layer of cartilage, a smooth tissue that minimizes friction and absorbs impact.
Arthritis disrupts this equilibrium. Pain, stiffness, swelling, and reduced range of motion may result from inflammation and cartilage breakdown, a poorly functioning immune system, and/or abnormal wear and tear.
Common Symptoms of Arthritis and Joint disorders
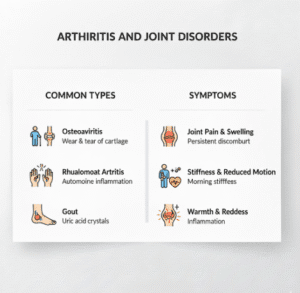
While symptoms may present differently for each type of arthritis, some are commonly seen across different types of the condition.
Joint discomfort is the most prevalent clinical presentation. It can occur either continuously or intermittently. Other common symptoms include morning or post-inactivity stiffness. Additionally, inflammation may occur, characterised by swelling, heat, and redness around the affected area.
If left untreated, the condition will worsen, leading to joint loss of strength and flexibility, which in turn will make even the simplest day-to-day tasks, such as walking, holding items, and using the stairs, much harder. The condition is also classified into different types.
Osteoarthritis
This is typically the most common type of arthritis and is known as ‘wear-and-tear arthritis’. Osteoarthritis occurs when the protective cartilage around joints is gradually eroded, leaving the underlying bones exposed to rub against one another.
The condition most commonly affects the knees, spine, and hands. Other risk factors include obesity, age, joint injuries, and repetitive movements that can strain the joints.
As the condition progresses, symptoms tend to worsen, and the affected person may start to feel pain during and after activities.
Rheumatoid Arthritis
This is also classified as an autoimmune disease, as the body’s immune system erroneously attacks and damages the joints. This results in prolonged inflammation that can erode the cartilage and bones and damage the surrounding tissue
Unlike other types of arthritis, rheumatoid arthritis affects joints symmetrically, such as both knees or both hands. In addition, it may cause a range of symptoms, including fatigue, fever, and unintentional weight loss.
Left untreated, rheumatoid arthritis can cause irreparable deformities of the joints. In addition, it can damage other vital organs, such as the lungs and heart.
Psoriatic Arthritis and Joint disorders
Psoriatic arthritis affects some patients with psoriasis, a long-term skin condition. It can cause pain, swelling, and stiffness in the ligaments, tendons, and joints.
Other symptoms include, but are not limited to, nail changes, lower back pain, and swollen toes or fingers. The severity of the disease can be inconsistent. However, to mitigate or prevent joint damage, it is essential to seek treatment early.
Gout
Gout is one type of inflammatory arthritis. It is caused by the deposition of sharp uric acid crystals in the joints and can affect other joints, but is primarily known for its effect on the big toe.
Gout attacks are unpredictable and can cause intense swelling, redness, pain, and other symptoms. Many factors can raise uric acid levels, including dehydration, certain foods, alcohol, and even genetics.
Other Joint Disorders
There are other forms of arthritis and joint disorders, such as juvenile idiopathic arthritis, infectious arthritis, and lupus-related arthritis, in addition to ankylosing spondylitis. They have their own specific features and treatment methods.
Causes and Risk Factors
Arthritis can develop for different reasons depending on which type you are considering. Common risk factors include ageing, genetics, joint injury, immune dysfunction, excess body weight, and repetitive joint stress.
Lifestyle factors such as physical inactivity, smoking, and poor nutrition can lead to symptoms being worse and also increase risk.
How Arthritis is Diagnosed
Diagnosis is based on the patient’s medical history, physical exam, and imaging tests and labs. X-rays and MRIs can detect joint damage. Also, blood tests can help show that the immune system is malfunctioning and that inflammatory forms of arthritis are present.
Diagnosis is essential for inflammatory arthritis, as without treatment, the disease can progress rapidly and be very damaging.
What Are the Options to Treat Arthritis
Most forms of arthritis do not have a cure, but treatment aims to control and reduce pain. Also, to improve function and help slow joint damage.
Medications can reduce pain and inflammation. Also, depending on the type of arthritis, inflammation-modifying drugs and biologic therapies are used.
Physical Therapy and Exercise
With regular low-impact exercise, the muscles surrounding the joints are strengthened. Also, the pain is decreased, and the overall movement is improved.
Lifestyle and Weight Management
The impact on knee and hip joints is alleviated by maintaining a healthy weight. Joint health is also aided by balanced nutrition and sufficient sleep.
Surgical Options
Joint repair or replacement surgeries are considered last resorts when conservative treatments are no longer effective.
Arthritis and Mental Health
Mobility restrictions, along with chronic pain, are liable to impact mental health. Those who have arthritis are particularly vulnerable to anxiety and depression, as well as social isolation.
Counselling, support groups, and stress management are essential to holistic care for emotional well-being.
Living with Arthritis
Arthritis requires long-term management and lifestyle adjustments. Many people effectively manage their symptoms with a combination of medical care, lifestyle changes, and physical activity.
Being educated about the condition allows people to make informed decisions and recognize when treatment adjustments are necessary.
Arthritis and Ageing
While arthritis is not a guaranteed outcome of ageing, ageing does considerably increase the risk of developing the disease. Increased time spent using particular joints, perennial shifts in muscle strength, and slowed cartilage repair are mechanisms that lead to increased joint failure with age.
Although the disease is highly prevalent in this demographic, arthritis is not something to merely suffer with. The care of arthritis is threefold and can lead to the alleviation of most problematic symptoms: appropriate medical treatment, maintenance of mobility, and supportive care.
The primary focus is the maintenance of joint flexibility and the minimization of pain through the strength and retention of muscle mass and the preservation of equilibrium in older adults, which ultimately reduces fall risk.
While it’s crucial to address the mechanism of ageing and the changes it produces, joint pain is never to be explained away with the deterministic phrase: “this is age-related.” A thorough medical check should always be conducted with pain that is persistent and leads to a reduction in functioning, and if this occurs, age should never be a mitigating factor.
The Role of Inflammation in Arthritis
Inflammation is a central characteristic of multiple forms of arthritis, especially autoimmune and inflammatory types such as rheumatoid arthritis, psoriatic arthritis, and gout. In autoimmune types, the immune system is overactive. It mistakenly attacks joint tissues, triggering a sustained immune response characterized by inflammation, pain, and joint stiffness.
Chronic inflammation is not only about swelling and pain. It can result in substantial destruction of the cartilage and, with it, the underlying bone, as well as the muscles and ligaments. In the absence of appropriate treatment, this can lead to joint deformities, loss of range of motion, and even total joint dysfunction.
Even in the case of osteoarthritis, which in the past has been classified as a wear-and-tear condition, low-grade inflammation contributes to cartilage loss and symptom progression. This has shifted the paradigm for understanding and treating osteoarthritis, with a greater focus on reducing inflammation and controlling mechanical stress on the joint.
Some forms of arthritis can cause systemic inflammation, which, in turn, can affect other organs. Inflammatory arthritis is associated with increased cardiovascular risk and systemic features, including fatigue, anemia, and osteoporosis. This is one of the reasons why arthritis is seen as a whole-body disorder rather than simply a problem which affects the joints.
The standard approach to controlling inflammation includes anti-inflammatory medications, physical exercise, stress management, and reducing joint load. Timely and continuous intervention is critical to minimizing the inflammatory processes and protecting the joints over time.
When to See a Doctor
Medical assessments are warranted if one experiences any degree of persistent joint pain, swelling, or stiffness, especially if the symptoms impact daily life and/or worsen. Early diagnosis, along with timely intervention, is crucial for preventing joint deterioration and improving quality of life.
Contact us if you need any medical information, guidance, or support.