Obesity is one of the most widely discussed—and often misunderstood—health conditions worldwide. It is frequently reduced to conversations about willpower, diet, or appearance, but medically, obesity is a complex, chronic disease influenced by biology, environment, behavior, and social factors.
Today, obesity affects people of all ages and backgrounds and is closely linked to several serious health conditions, including type 2 diabetes, high blood pressure (hypertension), heart disease, and arthritis. Understanding obesity as a medical condition—not a personal failure—is an important step toward effective and sustainable weight management.
This article explains what obesity is, why it happens, how it affects the body, its links to other chronic diseases, and what safe, evidence-based weight management looks like.
What Is Obesity?
Obesity is defined as an excess accumulation of body fat that increases the risk of health problems. In clinical settings, obesity is commonly screened using the Body Mass Index (BMI), which is calculated based on a person’s height and weight.
A BMI of 30 or higher generally falls into the obesity range. Doctors may further classify obesity based on severity, as higher levels of excess weight are associated with greater health risks. Although BMI does not directly measure body fat and has limitations—particularly in very muscular individuals—it remains a useful starting point for identifying obesity-related health concerns.
To gain a more accurate picture of health, healthcare providers often assess waist circumference, blood pressure, blood sugar levels, cholesterol levels, and a person’s overall medical history rather than relying on BMI alone.
Obesity as a Chronic Medical Condition
Modern medical research recognizes obesity as a chronic, relapsing condition, meaning it often develops gradually, persists over time, and may require long-term management. This classification reflects the fact that body weight is regulated by complex biological systems, not simply personal choices.
The brain, hormones, digestive system, and fat tissue all work together to regulate hunger, fullness, and energy balance. When these systems become dysregulated, the body may defend a higher weight, making weight loss difficult and weight regain common. This helps explain why many people experience repeated cycles of weight loss and regain despite strong efforts.
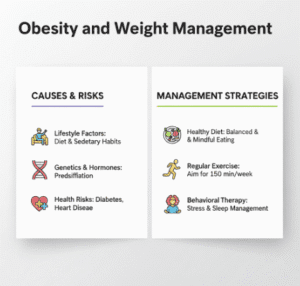
What Causes Obesity?
Obesity does not have a single cause. Instead, it develops from the interaction of biological, environmental, psychological, and social factors.
Biological and Genetic Influences
Genetics play a significant role in body weight. Some individuals are genetically predisposed to store fat more efficiently, experience stronger hunger signals, or have slower metabolic rates. These inherited traits can make weight gain more likely, especially in environments where high-calorie foods are readily available.
Hormones also play a critical role. Insulin, leptin, ghrelin, and cortisol influence appetite, fat storage, and energy use. Disruptions in these hormones—due to chronic stress, poor sleep, or underlying medical conditions—can promote weight gain and make weight loss harder to sustain.
Certain medical conditions, such as hypothyroidism, polycystic ovary syndrome (PCOS), and Cushing’s syndrome, can further contribute to weight gain by altering metabolism and hormone balance.
Environmental and Lifestyle Factors
Modern lifestyles often create conditions that favor weight gain. Sedentary work, prolonged screen time, limited physical activity, and easy access to calorie-dense foods all play a role. In many communities, healthy food options and safe spaces for exercise may be limited, making weight management even more challenging.
Sleep deprivation is another important factor. Inadequate sleep affects appetite-regulating hormones, increasing hunger and cravings while reducing feelings of fullness. Over time, this hormonal imbalance can contribute to gradual weight gain.
Psychological and Emotional Factors
Mental health and weight are closely connected. Conditions such as depression, anxiety, and chronic stress can influence eating behaviors, motivation, and energy levels. Emotional eating, binge eating, and using food as a coping mechanism are common responses to psychological distress and are strongly associated with obesity.
Weight stigma and repeated dieting failures can further worsen mental health, creating a cycle that makes long-term weight management more difficult.
Medications and Medical Treatments
Some medications can contribute to weight gain as a side effect. These include certain antidepressants, antipsychotic medications, steroids, and some treatments for diabetes. In these cases, weight gain is a physiological response rather than a lack of effort or discipline.
Health Risks Associated With Obesity
Obesity affects nearly every organ system in the body. The longer excess weight is present and the more severe it is, the greater the risk of developing chronic health conditions.
Obesity and Type 2 Diabetes
One of the strongest and most well-established links is between obesity and type 2 diabetes. Excess body fat, particularly around the abdomen, increases insulin resistance. This means the body’s cells do not respond effectively to insulin, causing blood sugar levels to rise.
Over time, insulin resistance can progress to prediabetes and eventually type 2 diabetes. Poorly controlled blood sugar can damage blood vessels and nerves, increasing the risk of heart disease, kidney disease, vision problems, and nerve damage.
Research shows that even modest, sustained weight loss can significantly improve insulin sensitivity and blood sugar control, reducing the risk of diabetes-related complications.
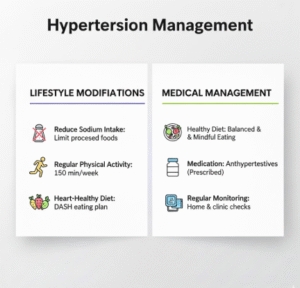
Obesity and High Blood Pressure (Hypertension)
Excess weight places additional strain on the heart and blood vessels. As body mass increases, the heart must work harder to pump blood, and blood vessels may become less flexible. Obesity also affects kidney function and fluid balance, both of which play a role in blood pressure regulation.
High blood pressure linked to obesity increases the risk of heart attack, stroke, heart failure, and kidney disease. Weight reduction has consistently been shown to lower blood pressure and, in some cases, reduce the need for long-term medication.
Obesity and Heart Disease
Obesity is a major risk factor for cardiovascular disease. It is associated with elevated cholesterol levels, higher triglycerides, chronic inflammation, and changes in blood vessel function. These factors contribute to the development of atherosclerosis, a condition in which arteries narrow due to plaque buildup.
As a result, people with obesity face a higher risk of coronary artery disease, heart attacks, and abnormal heart rhythms. The risk increases further when obesity is combined with diabetes or hypertension.
Obesity and Arthritis
Excess body weight places additional mechanical stress on joints, particularly the knees, hips, and lower back. Over time, this stress accelerates the breakdown of cartilage, increasing the risk of osteoarthritis.
Beyond mechanical strain, obesity is linked to low-grade systemic inflammation, which can worsen joint pain and stiffness. Studies show that even small reductions in body weight can significantly decrease joint pressure and improve mobility and pain levels.
Other Health Conditions Linked to Obesity
Obesity is also associated with sleep apnea, fatty liver disease, gallbladder disease, certain cancers, reproductive health issues, and reduced mobility. These conditions can affect quality of life and increase the risk of long-term disability if left unaddressed.
How Obesity Is Diagnosed
Diagnosing obesity involves more than measuring weight. Healthcare providers typically assess BMI alongside waist circumference, blood pressure, blood sugar levels, cholesterol levels, and liver function tests. A review of medications, lifestyle factors, and mental health history is also important.
This comprehensive approach helps identify underlying causes and obesity-related complications, allowing for more personalized management plans.
Understanding Weight Management
From a medical perspective, weight management focuses on reducing health risks and improving overall function, not achieving a specific body size. Research consistently shows that losing as little as 5 to 10 percent of body weight can lead to meaningful improvements in blood sugar control, blood pressure, joint pain, and cardiovascular health.
Safe and Evidence-Based Weight Loss Approaches
Safe weight loss emphasizes gradual, sustainable changes rather than rapid or extreme methods. Slow weight loss is more likely to be maintained and less likely to trigger metabolic adaptations that promote weight regain.
Regular physical activity plays an important role in weight management, but its benefits extend far beyond weight loss. Exercise improves insulin sensitivity, cardiovascular health, muscle strength, and mental well-being, even when weight changes are modest.
For some individuals, lifestyle changes alone may not be sufficient. Medical support can include structured weight management programs, behavioral therapy, prescription medications, or bariatric surgery in cases of severe obesity with related health complications. These options are typically considered within a comprehensive medical framework.
The Role of Mental and Emotional Health
Addressing mental and emotional health is a critical part of long-term weight management. Treating depression, anxiety, or chronic stress can improve energy levels, motivation, and overall quality of life. Psychological support can also help address disordered eating patterns and reduce the risk of relapse.
Living With Obesity and Reducing Stigma
Weight stigma remains a major barrier to care. Judgment and blame can discourage people from seeking medical help and can worsen both physical and mental health outcomes. A compassionate, medical approach to obesity recognizes it as a health condition deserving of evidence-based care and respect.
Progress does not require perfection. Small, consistent changes supported by healthcare professionals can lead to meaningful and lasting improvements in health.
When to See a Doctor
Medical guidance is especially important if weight gain is sudden or unexplained, if obesity is affecting daily activities, or if symptoms of diabetes, high blood pressure, or sleep apnea are present. Early intervention can help prevent long-term complications and improve outcomes.
Frequently Asked Questions (FAQs)
- Is obesity considered a disease or a lifestyle issue?
Obesity is recognized by medical organizations as a chronic disease. While lifestyle factors such as diet and physical activity play a role, obesity is also influenced by genetics, hormones, metabolism, mental health, medications, and environmental factors. Treating it solely as a lifestyle choice overlooks its biological and medical complexity. - Can someone be healthy and still have obesity?
Some individuals with obesity may not show immediate signs of conditions like diabetes or high blood pressure. However, obesity still increases the long-term risk of developing these health problems over time. Regular medical checkups help identify risks early and support proactive weight management focused on overall health rather than appearance. - How much weight loss is needed to see health benefits?
Research shows that losing just 5 to 10 percent of body weight can lead to meaningful improvements in blood sugar control, blood pressure, joint pain, and heart health. Significant health benefits can occur even without reaching a “normal” BMI. - Why is it so hard to lose weight and keep it off?
The body has complex systems that regulate hunger, fullness, and energy use. When weight is lost, hormonal and metabolic changes can increase appetite and reduce energy expenditure, making weight regain common. This is why obesity often requires long-term management rather than short-term dieting. - When should someone seek medical help for weight management?
Medical guidance is recommended if weight gain is rapid or unexplained, if obesity affects daily activities, or if conditions such as diabetes, high blood pressure, sleep apnea, or joint pain are present. A healthcare provider can help create a personalized, safe, and evidence-based management plan.
Key Takeaways:
Obesity is a chronic, complex medical condition influenced by genetics, hormones, environment, and mental health. It is closely linked to serious conditions such as diabetes, hypertension, heart disease, and arthritis.
Safe weight management focuses on improving health rather than rapid weight loss. With appropriate medical support, sustainable lifestyle changes, and a stigma-free approach, long-term health improvements are achievable.