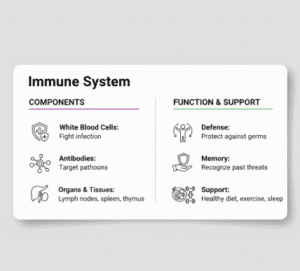
The immune system is the body’s defense network, protecting against infections, toxins, and abnormal cell growth. A healthy immune system efficiently identifies and neutralizes threats while maintaining balance to prevent overreactions, such as allergies or autoimmune conditions.
Immune system health is a topic of growing interest, particularly in the context of infections, chronic illnesses, and conditions like eczema or respiratory infections such as pneumonia. While genetics and age influence immunity, lifestyle, nutrition, medical interventions, and environmental exposures also play critical roles. Understanding how to support immunity both naturally and medically can reduce the risk of illness and improve overall health.
What Is the Immune System?
The immune system is a complex network of cells, tissues, and organs that defend the body against harmful invaders, including bacteria, viruses, fungi, and parasites. It is broadly divided into innate immunity and adaptive immunity.
Innate immunity is the first line of defense. It responds quickly to threats using physical barriers like skin and mucous membranes, as well as immune cells such as neutrophils and macrophages that attack pathogens immediately.
Adaptive immunity develops over time, providing targeted defense against specific pathogens. It involves specialized cells, including T lymphocytes and B lymphocytes, which produce antibodies. Adaptive immunity also creates immune memory, allowing the body to respond more effectively to future exposures.
Factors That Influence Immune Health
Immune function can be affected by multiple factors. Age is one of the most significant influences; as people age, immune responses often weaken, increasing susceptibility to infections like pneumonia. Genetics also play a role, influencing the number and activity of immune cells.
Nutrition, lifestyle, stress levels, sleep quality, and exposure to environmental toxins are additional modifiable factors that can strengthen or impair immunity. Chronic diseases, including diabetes, obesity, and autoimmune disorders, can reduce immune efficiency, making medical guidance essential for high-risk individuals.

Nutrition and Immunity
Nutrition is central to immune system health. The body requires vitamins, minerals, proteins, and healthy fats to produce immune cells, antibodies, and signaling molecules. Deficiencies in key nutrients can impair immune responses, increasing susceptibility to infections.
Vitamin C, found in citrus fruits and vegetables, supports white blood cell function and acts as an antioxidant. Vitamin D, synthesized through sunlight exposure and obtained from certain foods, modulates immune responses and reduces inflammation. Deficiencies in vitamin D have been linked to increased risk of respiratory infections.
Vitamin A supports the integrity of mucosal barriers, while zinc is critical for immune cell development and communication. Iron deficiency, often overlooked, can impair immune cell proliferation and function. Adequate protein intake provides amino acids needed for antibody and immune cell production.
A balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats is the foundation for optimal immunity. Conversely, excessive sugar, highly processed foods, and trans fats may impair immune responses and promote inflammation.
Lifestyle Factors That Boost Immunity
In addition to nutrition, lifestyle habits have a significant impact on immune health. Regular physical activity enhances circulation, allowing immune cells to travel more efficiently throughout the body. Moderate exercise has been shown to reduce the risk of infections, while excessive or intense exercise without adequate recovery can temporarily suppress immune function.
Sleep is critical for immune regulation. During sleep, the body produces cytokines, proteins that help fight infection and inflammation. Chronic sleep deprivation is associated with increased susceptibility to common infections, slower recovery, and reduced vaccine effectiveness.
Stress management is another key component. Chronic psychological stress elevates cortisol levels, which can suppress immune function, increase inflammation, and impair the body’s ability to fight infections. Mindfulness, meditation, yoga, and other stress-reduction strategies support immune health.
Avoiding tobacco and limiting alcohol intake are also essential. Smoking damages respiratory immune defenses, increasing the risk of infections like pneumonia, while excessive alcohol impairs immune cell function.
Common Conditions Linked to Impaired Immunity
An impaired or weakened immune system increases susceptibility to infections and certain chronic conditions.
Respiratory infections, including pneumonia, are more common in individuals with compromised immunity. Pneumonia can be bacterial or viral and poses significant risk in older adults, infants, and those with chronic illnesses.
Skin conditions such as eczema may reflect immune dysregulation. In eczema, the immune system overreacts to environmental triggers, leading to inflammation, itching, and skin barrier dysfunction. Supporting overall immunity, along with targeted dermatologic treatment, can reduce flare-ups.
Frequent infections, slow wound healing, or persistent fatigue may indicate underlying immune deficiencies, highlighting the importance of medical evaluation for individuals with recurrent illnesses.
Medical Approaches to Support Immunity
While nutrition and lifestyle are foundational, certain medical interventions can strengthen immunity in specific contexts. Vaccinations are among the most effective medical strategies for preventing infections. Vaccines prime the adaptive immune system to recognize and combat pathogens, reducing the risk of serious illness from diseases such as influenza, pneumonia, and COVID-19.
For individuals with chronic illness, autoimmune conditions, or immunodeficiencies, medical management may include supplementation of essential nutrients like vitamin D, vitamin B12, or iron. These interventions should be guided by laboratory testing to correct deficiencies without causing toxicity.
In cases of recurrent or severe infections, healthcare providers may evaluate for underlying immune system disorders. In rare instances, treatments such as immunoglobulin therapy, targeted biologics, or other immune-modulating medications may be indicated.
Natural Immune Support Strategies
Beyond diet and medical interventions, several natural strategies can support immune health:
Probiotics may improve gut health, which is closely linked to immune function. The gut microbiome influences the development and regulation of immune cells, and a diverse, balanced microbiome enhances defense against pathogens. Fermented foods, yogurt, and probiotic supplements are potential sources of beneficial bacteria.
Hydration supports all bodily functions, including immune cell transport and removal of toxins. Adequate water intake is essential for maintaining mucosal barriers in the respiratory and gastrointestinal tracts, which are first lines of defense against infection.
Sunlight exposure not only promotes vitamin D synthesis but may also have direct immune-regulating effects. Moderate sunlight exposure, combined with protective measures against excessive UV radiation, can contribute to immune health.
Herbal supplements such as echinacea, garlic, and elderberry have been studied for immune support. While evidence varies, some individuals may benefit from these as adjuncts to a balanced diet and lifestyle, under medical supervision to avoid interactions with medications.
Immune Health Across Life Stages
Immune function changes across the lifespan. Infants and young children rely on maternal antibodies initially, with their own adaptive immunity developing over time. Proper nutrition, vaccinations, and avoidance of unnecessary antibiotic overuse are critical in early life.
Adults face challenges from lifestyle factors, chronic illness, and environmental exposures. Maintaining a balanced diet, regular exercise, stress management, and adherence to vaccination schedules are essential for lifelong immune resilience.
Older adults often experience immunosenescence, a natural decline in immune function with age. This increases susceptibility to infections, including pneumonia, influenza, and shingles. Targeted strategies, including vaccinations, nutritional support, and medical supervision, are essential in this population.
Monitoring Immune Health
While there is no single test to measure overall immunity, certain laboratory tests can indicate immune function or nutrient deficiencies. Complete blood counts, immunoglobulin levels, and nutrient panels (vitamin D, B12, iron, zinc) provide insights into immune status.
Medical evaluation is warranted for individuals with frequent infections, delayed recovery from illness, persistent fatigue, or immune-related conditions such as eczema. Early intervention can prevent complications and support long-term health.
Special Considerations for Immunocompromised Individuals
Certain populations have compromised immunity due to medical conditions, treatments, or age. This includes individuals undergoing chemotherapy, taking immunosuppressive medications, living with HIV, or recovering from major surgery. For these individuals, even common infections can be severe, requiring preventive strategies and careful medical oversight.
Vaccinations, prophylactic treatments, strict hygiene measures, and timely medical intervention are critical. Nutritional and lifestyle interventions remain beneficial, though they are often used in conjunction with medical therapies to support immune resilience.
Integrating Natural and Medical Approaches
Optimal immune support involves a combination of natural and medical strategies. Lifestyle habits like balanced nutrition, exercise, sleep, and stress management provide a foundation, while vaccinations, supplementation, and targeted therapies address specific deficiencies or vulnerabilities.
Avoiding overreliance on supplements or unproven remedies is important. Evidence-based strategies, guided by healthcare providers, ensure safe and effective immune support.
Common Misconceptions About Immunity
Several myths surround immune health. Taking megadoses of vitamins or supplements does not guarantee protection and can sometimes cause harm. Over-the-counter immune boosters are not substitutes for vaccinations or healthy lifestyle habits.
Similarly, antibiotics are ineffective against viral infections and their misuse can impair gut microbiota and immune regulation. Understanding the limits and appropriate use of medical interventions is critical for true immune support.
When to Seek Medical Advice
Medical evaluation is important when individuals experience frequent infections, persistent fatigue, slow recovery from illness, worsening eczema, or any severe symptoms. Laboratory testing can identify deficiencies or underlying immune disorders.
Early consultation allows for targeted interventions, including nutrient correction, medical therapies, or vaccinations, reducing the risk of serious infections such as pneumonia.
Frequently Asked Questions (FAQs)
- Can you really “boost” your immune system?
The immune system cannot be simply “boosted” like turning up a switch. Instead, immune health is about balance and proper function. Healthy lifestyle habits, adequate nutrition, and appropriate medical care help the immune system work efficiently without becoming overactive, which could lead to allergies or autoimmune conditions. - Do supplements improve immunity if you eat a healthy diet?
For most healthy individuals with a balanced diet, supplements are not necessary. However, deficiencies in nutrients such as vitamin D, vitamin B12, iron, or zinc can impair immune function. In these cases, supplementation guided by blood tests and medical advice can be beneficial. Excessive or unnecessary supplementation may cause harm. - How does sleep affect immune health?
Sleep plays a critical role in immune regulation. During sleep, the body produces cytokines and other immune mediators needed to fight infections and inflammation. Chronic sleep deprivation weakens immune responses, increases infection risk, and may reduce vaccine effectiveness. - Are natural remedies like probiotics or herbal supplements effective?
Some natural approaches, such as probiotics, may support immune health by improving gut microbiome balance, which influences immune regulation. Herbal supplements like echinacea or elderberry may offer modest benefits for some individuals, but evidence varies. These should be used cautiously and not as substitutes for medical care or vaccinations. - When should someone be concerned about a weak immune system?
Frequent infections, slow wound healing, persistent fatigue, worsening eczema, or recurrent respiratory illnesses such as pneumonia may signal impaired immune function. Individuals experiencing these symptoms should seek medical evaluation to identify underlying causes and receive appropriate treatment.
Key Takeaways
The immune system is a complex and dynamic network that protects the body from infections and maintains overall health. Immune health is influenced by genetics, age, nutrition, lifestyle, medical conditions, and environmental factors.
Supporting immunity naturally includes a nutrient-rich diet, adequate sleep, regular exercise, stress management, hydration, and moderate sun exposure. Medical strategies, including vaccinations, supplementation, and targeted therapies, are essential in high-risk populations or when deficiencies exist.
A strong immune system reduces the risk of infections, supports recovery, and improves quality of life. Individuals with chronic illnesses, frequent infections, eczema, or other immune-related conditions should work closely with healthcare providers to optimize immune function safely and effectively.