Vitamin and mineral deficiencies are surprisingly common, even in well-nourished populations. Among the most frequently diagnosed are deficiencies in vitamin D, vitamin B12, and iron. These nutrients are essential for energy production, immune function, nerve health, and overall well-being. When levels are low, the body can experience fatigue, weakness, mood changes, and a range of physical and cognitive symptoms.
Because these deficiencies are common yet often subtle, many people go years without realizing they are affected. Early recognition through proper testing and timely treatment can prevent complications and restore health. Vitamin and mineral deficiencies are also closely linked with conditions such as anemia, thyroid disorders, fatigue, and poor bone health, making their detection essential for overall medical care.
This article explains the causes, symptoms, diagnostic tests, and treatment options for vitamin D, B12, and iron deficiencies.

Vitamin D Deficiency
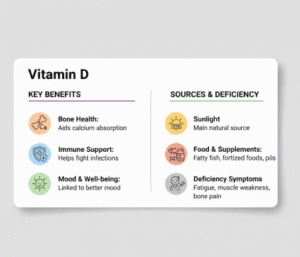
Vitamin D is a fat-soluble vitamin essential for bone health, immune function, and cell growth. It is unique because the body can produce it when the skin is exposed to sunlight, although dietary sources also contribute.
Causes of Vitamin D Deficiency
Vitamin D deficiency can develop due to limited sun exposure, darker skin pigmentation, obesity, aging, or malabsorption disorders such as celiac disease or inflammatory bowel disease. Certain medications, such as steroids, can also reduce vitamin D levels. Individuals living in northern latitudes or who spend most of their time indoors are particularly at risk.
Symptoms of Vitamin D Deficiency
Symptoms are often subtle at first and may include fatigue, muscle weakness, bone pain, and frequent infections. Chronic deficiency can lead to bone loss, osteoporosis, or rickets in children. Mood disturbances, including low mood or depressive symptoms, have also been linked to low vitamin D levels.
Testing and Diagnosis
Vitamin D status is assessed with a blood test measuring 25-hydroxyvitamin D levels. Optimal levels vary slightly among experts, but deficiency is generally defined as below 20 ng/mL, while insufficiency is considered between 21–29 ng/mL.
Treatment
Treatment involves increasing sun exposure, dietary intake of vitamin D-rich foods (fatty fish, fortified dairy, eggs), and supplementation. The dosage and duration depend on the severity of deficiency and individual risk factors. Regular monitoring is recommended to ensure adequate levels without exceeding safe limits.
Vitamin B12 Deficiency
Vitamin B12 is a water-soluble vitamin crucial for red blood cell formation, nerve function, and DNA synthesis. The body relies on dietary intake, mainly from animal products, making vegetarians and vegans particularly vulnerable to deficiency.
Causes of B12 Deficiency
B12 deficiency can result from inadequate dietary intake, poor absorption due to gastrointestinal conditions (such as pernicious anemia, celiac disease, or gastritis), certain medications (like metformin or proton pump inhibitors), and age-related changes in stomach acid production.
Symptoms of B12 Deficiency
B12 deficiency can manifest as fatigue, weakness, tingling or numbness in the hands and feet, memory problems, mood changes, and pale or jaundiced skin. Severe or prolonged deficiency can lead to irreversible nerve damage if left untreated.
Testing and Diagnosis
B12 status is typically assessed with a blood test measuring serum B12 levels. Additional tests, such as methylmalonic acid and homocysteine levels, may help detect early deficiency or confirm functional deficiency even when serum B12 appears normal.
Treatment
Treatment involves oral supplements or intramuscular B12 injections, depending on the severity and cause of deficiency. Individuals with absorption issues may require lifelong supplementation. Monitoring ensures that levels return to normal and symptoms improve.
Iron Deficiency
Iron is a mineral essential for oxygen transport, energy production, and numerous enzymatic reactions in the body. Iron deficiency is the most common nutritional deficiency worldwide.
Causes of Iron Deficiency
Iron deficiency can develop due to inadequate dietary intake, poor absorption (for example, in celiac disease or after gastrointestinal surgery), increased demand (pregnancy, growth spurts), or chronic blood loss (menstruation, gastrointestinal bleeding, or frequent UTIs with hematuria). Certain medications, like NSAIDs, can increase the risk of bleeding and contribute to iron deficiency.
Symptoms of Iron Deficiency
Iron deficiency often causes fatigue, weakness, pale skin, shortness of breath, dizziness, brittle nails, and headaches. In advanced cases, it may lead to iron-deficiency anemia, resulting in rapid heart rate, cold intolerance, and reduced exercise tolerance. Cognitive difficulties, such as poor concentration or memory problems, are also common.
Testing and Diagnosis
Iron status is assessed through blood tests including serum ferritin, serum iron, total iron-binding capacity (TIBC), and hemoglobin levels. Ferritin is the most sensitive marker of iron stores, while hemoglobin indicates whether anemia has developed.
Treatment
Iron deficiency is treated with oral iron supplements, dietary modification (red meat, legumes, dark leafy greens, fortified cereals), and addressing underlying causes of blood loss. In severe cases or when oral iron is poorly tolerated, intravenous iron may be required. Regular monitoring ensures that iron stores are restored and maintained.
Interconnections Between Deficiencies
Vitamin D, B12, and iron deficiencies often coexist, particularly in individuals with chronic illnesses, thyroid disorders, gastrointestinal malabsorption, or restrictive diets. Each deficiency can amplify fatigue, reduce energy, and affect mood and cognitive function. Addressing all potential deficiencies is critical for holistic recovery.
When to See a Doctor
Medical evaluation is warranted if fatigue, weakness, pale skin, numbness, or mood changes persist despite adequate rest and nutrition. People with risk factors such as vegetarian or vegan diets, chronic illnesses, thyroid disorders, frequent UTIs, gastrointestinal disorders, pregnancy, or heavy menstruation should consider screening.
Early detection allows for targeted supplementation and prevents complications such as anemia, bone weakening, or nerve damage.
Lifestyle and Dietary Support
Alongside medical treatment, lifestyle and dietary strategies can help prevent and correct deficiencies.
- For vitamin D: safe sun exposure, fortified foods, fatty fish, and supplementation as advised.
- For B12: inclusion of animal products, fortified plant-based foods, or supplementation.
- For iron: combination of iron-rich foods with vitamin C sources to enhance absorption, avoiding excessive tea or coffee at mealtimes.
Addressing dietary patterns, sleep, and stress also supports overall nutrient utilization and energy levels.
Frequently Asked Questions (FAQs)
- How do I know if I have a vitamin or mineral deficiency?
Deficiencies often develop slowly, so symptoms may be subtle. Common signs include fatigue, weakness, pale skin, mood changes, tingling in the hands or feet, and poor concentration. Blood tests are the most reliable way to confirm deficiency in vitamin D, B12, or iron. - Who is at higher risk for these deficiencies?
People at higher risk include those with chronic illnesses, thyroid disorders, gastrointestinal conditions, heavy menstrual bleeding, frequent urinary tract infections, restrictive diets (vegetarian or vegan), pregnancy, or limited sun exposure. Age and certain medications can also increase risk. - Can diet alone correct these deficiencies?
Diet plays a key role but may not be sufficient in all cases. Vitamin D may require supplementation if sunlight exposure is limited, B12 supplementation is often needed for vegetarians or those with absorption issues, and iron supplements may be necessary for those with chronic blood loss or severe deficiency. - What tests are used to detect these deficiencies?
- Vitamin D: 25-hydroxyvitamin D blood test
- Vitamin B12: Serum B12, with possible methylmalonic acid or homocysteine testing
- Iron: Serum ferritin, serum iron, total iron-binding capacity (TIBC), and hemoglobin levels
- How are vitamin D, B12, and iron deficiencies treated?
Treatment typically involves supplementation, dietary improvements, and addressing underlying causes. Vitamin D and B12 may be given orally or via injections in severe cases. Iron supplementation can be oral or intravenous depending on tolerance and severity. Regular monitoring ensures nutrient levels are restored safely.
Key Takeaways
Vitamin D, B12, and iron deficiencies are common but often subtle, with symptoms including fatigue, weakness, mood changes, and cognitive difficulties. Early recognition through testing and proper treatment can prevent complications such as anemia, nerve damage, and bone loss.
People with thyroid disorders, recurrent infections like UTIs, restrictive diets, or chronic illnesses are particularly at risk. Treatment combines supplementation, dietary improvements, and addressing underlying causes. With appropriate care, nutrient levels can be restored, and overall health improved.