Chronic kidney disease (CKD) is a long-term condition that affects millions of people worldwide, yet it often goes unnoticed in its early stages. Many individuals with CKD feel well for years before symptoms appear, allowing kidney damage to progress silently.
The kidneys play a vital role in filtering waste, balancing fluids and electrolytes, regulating blood pressure, and supporting red blood cell production. When kidney function declines, these processes are disrupted, increasing the risk of serious health complications.
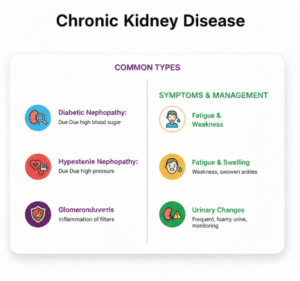
Chronic kidney disease is closely linked to diabetes, high blood pressure (hypertension), and recurrent urinary tract infections (UTIs). In fact, diabetes and hypertension are the leading causes of CKD globally. Understanding how CKD develops, recognizing early symptoms, and managing risk factors can significantly slow disease progression and improve quality of life.

What Is Chronic Kidney Disease?
Chronic kidney disease is defined as a gradual loss of kidney function that lasts for three months or longer. Unlike acute kidney injury, which occurs suddenly and may be reversible, CKD develops slowly and is usually permanent.
Healthy kidneys filter excess fluids, waste products, and toxins from the blood, which are then excreted in urine. They also help regulate blood pressure, maintain bone health, and support hormone production. When kidney function declines, waste products and fluids can build up in the body, leading to widespread effects.
CKD ranges from mild kidney damage with few symptoms to severe kidney failure requiring dialysis or transplantation.
How Common Is Chronic Kidney Disease?
CKD is one of the most common chronic conditions worldwide. Many people are unaware they have it because early-stage disease often causes no noticeable symptoms.
Risk increases with age, but CKD can affect younger individuals, particularly those with diabetes, hypertension, autoimmune conditions, or a history of recurrent kidney infections.
Early detection is critical, as timely management can slow progression and reduce complications.
Stages of Chronic Kidney Disease
Chronic kidney disease is classified into five stages based on a measure called the estimated glomerular filtration rate (eGFR), which reflects how well the kidneys are filtering blood.
Stage 1: Kidney Damage With Normal or High Function
In stage 1, kidney damage is present, but overall kidney function remains near normal. People at this stage often have no symptoms, and CKD may only be detected through abnormal urine tests or imaging studies.
Management focuses on identifying the cause of kidney damage and controlling risk factors to prevent progression.
Stage 2: Mild Decrease in Kidney Function
Stage 2 involves a mild reduction in kidney function. Symptoms are still uncommon, but subtle changes such as mild fatigue or changes in urination may begin to appear.
At this stage, addressing conditions like diabetes and hypertension is essential to protect remaining kidney function.
Stage 3: Moderate Kidney Damage
Stage 3 is divided into two sub-stages and represents a moderate decline in kidney function. Symptoms may become more noticeable and include fatigue, swelling in the legs or ankles, changes in urination, and difficulty concentrating.
This stage is often when CKD is first diagnosed, especially if blood tests reveal rising creatinine levels or declining eGFR.
Stage 4: Severe Kidney Damage
In stage 4, kidney function is significantly reduced. Waste products accumulate more rapidly, and symptoms may include nausea, loss of appetite, persistent swelling, muscle cramps, and worsening fatigue.
Care at this stage focuses on slowing progression, managing complications, and preparing for possible kidney replacement therapy.
Stage 5: Kidney Failure
Stage 5, also known as end-stage kidney disease, occurs when the kidneys can no longer meet the body’s needs. Dialysis or kidney transplantation becomes necessary to sustain life.
Not everyone with CKD progresses to this stage, especially with early detection and appropriate management.
Symptoms of Chronic Kidney Disease
One of the challenges of CKD is that symptoms often appear late in the disease course. Early stages may cause no noticeable signs, allowing kidney damage to progress silently.
As kidney function declines, symptoms may include persistent fatigue, swelling in the feet or ankles, changes in urination frequency or appearance, shortness of breath, nausea, poor appetite, itching, and difficulty sleeping.
Because these symptoms are non-specific, they are often mistaken for other conditions or aging, delaying diagnosis.
Chronic Kidney Disease and Fatigue
Fatigue is one of the most common and disabling symptoms of CKD. Reduced kidney function affects red blood cell production, leading to anemia, which decreases oxygen delivery to tissues.
Toxin buildup and chronic inflammation further contribute to persistent tiredness that is not relieved by rest.
Causes of Chronic Kidney Disease
CKD usually develops due to long-standing conditions that place continuous strain on the kidneys.
Diabetes and Chronic Kidney Disease
Diabetes is the leading cause of chronic kidney disease. Elevated blood sugar damages the tiny blood vessels in the kidneys, impairing their ability to filter waste effectively.
Over time, this damage leads to diabetic kidney disease, also known as diabetic nephropathy. Poor blood sugar control significantly increases the risk of progression, while early management can slow or prevent kidney damage.
Hypertension and Kidney Damage
High blood pressure is both a cause and a consequence of chronic kidney disease. Elevated blood pressure damages blood vessels in the kidneys, reducing blood flow and impairing filtration.
As kidney function declines, fluid and sodium balance are disrupted, which can further raise blood pressure. This creates a harmful cycle that accelerates kidney damage if not addressed.
Recurrent UTIs and Kidney Disease
Frequent or untreated urinary tract infections can increase the risk of chronic kidney damage, particularly when infections spread to the kidneys, a condition known as pyelonephritis.
Repeated kidney infections cause scarring, which reduces functional kidney tissue over time. This risk is higher in individuals with structural abnormalities of the urinary tract or conditions that impair immune function.
Other Causes of CKD
Other contributors include autoimmune diseases, chronic inflammation, inherited kidney disorders, long-term use of certain medications, and prolonged obstruction of the urinary tract.
In many cases, CKD results from a combination of factors rather than a single cause.
How Chronic Kidney Disease Is Diagnosed
Diagnosis involves blood and urine tests that assess kidney function and detect early signs of damage. Blood tests measure creatinine levels and estimate glomerular filtration rate, while urine tests look for protein or blood.
Imaging studies may be used to evaluate kidney size and structure. Identifying the underlying cause is essential for guiding treatment and slowing progression.
Managing Chronic Kidney Disease
Although CKD cannot usually be reversed, appropriate management can slow progression and reduce complications.
Blood Sugar Control
For individuals with diabetes, maintaining stable blood sugar levels is one of the most effective ways to protect kidney function. Good glucose control reduces damage to kidney blood vessels and lowers the risk of progression.
Blood Pressure Management
Controlling blood pressure is critical in all stages of CKD. Even modest reductions in blood pressure can significantly slow kidney damage and reduce cardiovascular risk.
Blood pressure management often involves a combination of lifestyle measures and medication.
Managing UTIs and Preventing Infections
Prompt treatment of urinary tract infections helps prevent kidney involvement and long-term scarring. Individuals with recurrent UTIs may require further evaluation to identify underlying causes.
Maintaining hydration and regular medical follow-up supports urinary tract health.
Monitoring and Medical Follow-Up
Regular monitoring allows healthcare providers to track kidney function, adjust treatments, and detect complications early. This includes routine blood tests, urine tests, and blood pressure checks.
Living With Chronic Kidney Disease
Living with CKD often requires long-term lifestyle adjustments and ongoing medical care. Many people with early-stage CKD live full, active lives with appropriate management.
Education, adherence to treatment plans, and regular follow-up play a key role in preserving kidney function and quality of life.
When to See a Doctor
Medical evaluation is important if there are risk factors such as diabetes, hypertension, recurrent UTIs, or a family history of kidney disease. Symptoms such as swelling, persistent fatigue, changes in urination, or unexplained nausea should also prompt evaluation.
Early diagnosis provides the best opportunity to slow disease progression.
Frequently Asked Questions (FAQs)
- What are the earliest signs of chronic kidney disease?
Early-stage chronic kidney disease often causes no noticeable symptoms. As kidney function begins to decline, subtle signs such as mild fatigue, changes in urination, or swelling in the ankles may appear. Because symptoms are often absent early on, CKD is frequently detected through routine blood and urine tests. - Can chronic kidney disease be reversed?
In most cases, chronic kidney disease cannot be reversed because kidney damage is usually permanent. However, early diagnosis and proper management can significantly slow disease progression, preserve remaining kidney function, and reduce the risk of complications. - How are diabetes and high blood pressure linked to CKD?
Diabetes and high blood pressure damage the small blood vessels in the kidneys over time, reducing their ability to filter waste effectively. Together, these conditions are the leading causes of CKD worldwide. Controlling blood sugar and blood pressure is essential for protecting kidney health. - Can recurrent urinary tract infections cause kidney disease?
Yes. Repeated or untreated UTIs can spread to the kidneys and cause scarring, which may lead to chronic kidney disease over time. This risk is higher when infections are frequent, severe, or involve the kidneys directly. - How is chronic kidney disease managed long term?
Management focuses on slowing progression and preventing complications. This includes controlling blood pressure and blood sugar, treating infections promptly, monitoring kidney function regularly, and following medical advice tailored to the stage and cause of CKD.
Key Takeaways
Chronic kidney disease is a common, progressive condition that often develops silently. It is strongly linked to diabetes, high blood pressure, and recurrent urinary tract infections.
Although CKD cannot usually be cured, early detection and effective management can significantly slow progression, reduce complications, and improve long-term outcomes.