Eczema and Psoriasis Treatment Guide
Millions of people worldwide are affected by two skin conditions, eczema and psoriasis. The two skin conditions can appear very similar to the naked eye, but have different root causes, symptoms and treatment protocols. Both conditions can cause skin changes and emotional distress to the sufferer. They also tend to have episodes of worsening symptoms and periods when symptoms are under control.
Differentiating the symptoms of the two skin conditions can help identify the condition, which in turn can facilitate timely and appropriate care to manage it effectively.

Understanding Chronic Skin Conditions
Chronic inflammatory skin conditions can occur when the skin’s protective barrier is disrupted and when the skin’s immune system begins to behave unusually. The skin is the body’s protective barrier against the environment, and, to give atopic dermatitis and psoriasis some context, both involve the skin’s immune system.
Psoriasis and eczema are both inflammatory conditions that are not contagious, but can significantly impact the sufferer’s quality of life. Both situations involve different immune mechanisms and skin responses.
What Is Eczema?
Atopic dermatitis, or eczema, is a chronic condition characterized by dehydrated, itchy, and inflamed skin. The inflamed skin can also appear very swollen. The skin condition can develop at any age, but is common in childhood. Eczema occurs more often in people with allergies or asthma, or in family members with allergies, asthma, or hay fever.
Eczema is characterized by a compromised dermal barrier, leading to increased moisture loss and allowing irritants to enter more readily. Moisture loss is accompanied by inflammation and moisture-balancing irritants, resulting in intense pruritus. An inflammatory feedback loop ensues.
Common Symptoms of Eczema
Eczema can present in many ways. In terms of presentation, the main differentiating factors are age, skin type, and the degree of eczema. Presentation of eczema typically includes the following. First, there is a zone of dry, delicate skin surrounded by an erythematous halo.
Next, a persistent itch accompanies the skin changes. Affected skin eventually develops a zone of inflammation, which includes swelling and the formation of rough and scaly spots. In more severe cases, the affected or broken skin can become superinfected with bacteria.
The sufferer was inflicted with a severe disability due to eczema. Weakened, irritated skin can lead to an itch that intensifies during sleep. That eventually leads to more inflammation. Only a temporary cessation of discomfort is to be expected.
Eczema is of great concern because it can affect the cheeks and scalp of infants and young children. In children and adults, the inflamed skin is most commonly found in the folds of the elbows and knees.

Why Flare-ups of Eczema Occur
Environmental and lifestyle factors commonly aggravate eczema. Dry air, moisture-sapping soaps and detergents, certain fabrics, allergens, stress, and even thermoregulatory sweating can lead to moisture loss and serve as environmental triggers.
Food allergens can play a role, although they are less commonly a trigger in older age groups. In assessing eczema, it’s essential to remember that people with eczema can have different outflow and environmental triggers that lead to its presentation, in the absence of a particular environment. This is an essential part of eczema and its presentation.
What Is Psoriasis?
Psoriasis is a chronic autoimmune condition. In this condition, the body’s immune system forces skin cells to multiply faster than is considered normal. Instead of a normal cell shedding cycle of several weeks, skin cells shed every few days. This process causes the skin to shed and build up, resulting in scaly patches.
Psoriasis can arise at any age; however, it is most likely to occur in adulthood. Psoriasis differs from conditions such as eczema in that it is not primarily associated with allergies, and it does not commonly cause severe itching, though mild itching can occur.
Common Symptoms of Psoriasis
Psoriatic skin is a disease of the skin in the form of definite patches of skin that are diseased, which have scaling that is silvery and white. Specifically, the disease manifests most commonly on the elbows, knees, scalp, and lower back, and can affect the nails.
Also, other possible symptoms of psoriasis and skin disease include dry/or cracked, or bleeding skin. Some people can even have nails that exhibit weakening, separation from the nails, and/or a deteriorated nail bed. Others may experience pain or stiffness in joints affected by psoriatic arthritis.
Psoriasis symptoms can range from mild to severe. Psoriasis can also have periods of active symptoms and periods of no symptoms.
Eczema and Psoriasis: Differences between Eczema and Psoriasis
- While conditions like eczema and psoriasis cause skin inflammation and result in changes to the skin, several symptoms can help to distinguish the two.
- Eczema commonly includes dry skin and more than moderate rough itching, and it usually comprises spurious patches. Common triggers for eczema are environmental. Eczema also begins in early childhood.
- Psoriasis often appears as noticeably thicker plaques with defined edges and scale. By ramping up immune dysfunction, the condition may also involve the joints and other systems.
- An accurate and timely clinical diagnosis is imperative, as there is a disparity in the conditions’ therapeutic approaches.
Causes and Risk Factors
Eczema is a syndrome with presumed multifactorial etiology resulting from a complex interplay of genetic, immunologic perturbations, and environmental factors. Patients with eczema frequently present with a genetic alteration that impairs the functionality of the skin barrier, thereby augmenting trans-epidermal water loss and resulting in dry, itchy skin.
Psoriasis is a skin condition driven by immune dysfunction, with a specific focus on culprit T lymphocytes that orchestrate abnormal epidermal proliferation. Genetic predisposition is predominant, and psoriatic disease is often familial.
Potential triggers for psoriasis may include, but are not limited to, infections, emotional stress, skin trauma, cigarette smoking, alcoholic beverages, and other specific therapeutic agents.
How Eczema and Psoriasis are Diagnosed
These conditions are generally diagnosed based on a clinical evaluation, including a history of medical illness. In some instances, a skin biopsy might be performed to confirm the diagnosis or exclude other underlying conditions associated with psoriasis.
Given the potential for clinical symptom overlap, particularly in less pronounced cases, a dermatologist’s clinical judgement is often invaluable.
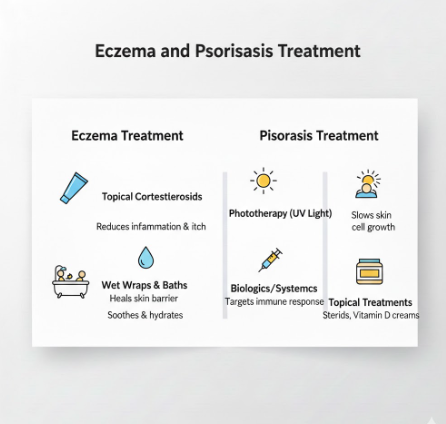
Treatment Options for Eczema
Eczema management strategies aim to permanently restore the skin barrier function, control inflammation, and manage pruritus symptoms.
Moisturizers should form the backbone of eczema care due to their role in skin hydration. Additionally, potential skin inflammation during eczema flare-ups is addressed with corticosteroid ointments. Regular use of moisturizers is thus essential, since corticosteroid ointments do little to maintain skin hydration over the long term.
In cases of severe eczema, calcineurin inhibitors and oral medications may be necessary. In moderate-to-severe cases, recent biologic therapies may also be used.
Along with the above treatments, long-term management is aided by avoiding potential triggers and using skin care products free of harsh chemicals.
Eczema and psoriasis are both chronic inflammatory skin diseases, and their impacts are both physical and emotional. The severity and extent of psoriasis also dictate which treatments should be used and when: for mild to moderate disease, topical treatments such as corticosteroid ointments and vitamin D analogues are preferred, while phototherapy can be used for more widespread disease. As with other moderate-to-severe diseases, when joints are affected, systemic medications should be used in addition to biologic therapies targeting specific immune pathways.
Effective phototherapy involves shorter, more frequent sessions at first. Visible skin lesions often lead to low self-esteem and can affect an individual’s social interactions and overall mental health.
In addition, chronic itching or pain is not only disruptive to sleep but can also increase stress, which triggers an exacerbation of the disease. Disrupted sleep can lead to further stress, which exacerbates underlying disease. Focusing on emotional well-being is thus essential in these chronic inflammatory skin diseases.
Living With Eczema or Psoriasis
Chronic skin conditions require personalized attention and ongoing adjustments in care. For many, identifying the early warning signs of flare-ups and adjusting management strategies accordingly becomes a necessary routine.
A Combination of systematically adjusting skin care regimens, practicing stress management, and keeping regular healthcare appointments helps keep the condition stable.
When to See a Doctor
Assessment of the skin by a General Practitioner is warranted when symptoms are chronic, progressively deteriorating, or limit the patient’s ability to engage in daily life. Quick attention is also warranted if there are signs of infection, such as increased pain, redness, warmth, and oozing.
Complications and discomfort of the skin can be chronic, and mental distress can also become more entrenched if there are no effective strategies put in place, so timely diagnosis is essential.
Contact us if you need any medical information, guidance, or support.