Irritable Bowel Syndrome (IBS) is one of the most common gastrointestinal disorders worldwide, affecting up to 10–15% of adults. Despite its prevalence, IBS is often underdiagnosed or misdiagnosed, and many people live for years without knowing they have it. IBS is a functional disorder, meaning the gut appears normal on medical tests but does not function properly. It is characterized by symptoms such as abdominal pain, bloating, constipation, diarrhea, or alternating bowel habits, which can significantly affect quality of life.
IBS is closely linked with anxiety, stress, gastroesophageal reflux disease (GERD), and sometimes sensitivities to medications or certain foods. While it does not cause permanent damage to the intestines or increase cancer risk, IBS can be chronic and disruptive, making symptom management essential.
This article provides a comprehensive overview of IBS, including its causes, symptoms, triggers, diagnosis, dietary strategies, medications, and lifestyle approaches for long-term management.

What Is IBS?
IBS is classified as a functional gastrointestinal disorder because the intestines do not work as they should, even though they appear normal under a microscope or imaging test. This contrasts with inflammatory bowel diseases (IBD) like Crohn’s disease or ulcerative colitis, which cause visible damage to the gut lining.
IBS affects the communication between the brain and the gut, a connection known as the gut-brain axis. This can lead to abnormal gut motility, increased sensitivity to intestinal pain, and changes in digestive secretions.
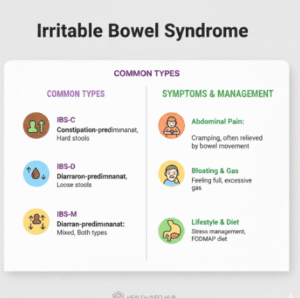
IBS is divided into subtypes based on bowel habits:
- IBS with constipation (IBS-C): Hard, infrequent stools
- IBS with diarrhea (IBS-D): Loose, watery stools
- Mixed IBS (IBS-M): Alternating constipation and diarrhea
Symptoms often fluctuate and may worsen during periods of stress, dietary changes, or illness.
Symptoms of IBS
IBS symptoms can vary in intensity and frequency. Some individuals experience mild discomfort, while others have symptoms severe enough to interfere with work, social activities, and daily routines.
Common symptoms include:
- Abdominal pain or cramping, often relieved by bowel movements
- Changes in stool frequency and form (diarrhea, constipation, or both)
- Bloating, gas, and a feeling of fullness
- Urgency or difficulty controlling bowel movements
- Mucus in the stool
- Fatigue, sleep disturbances, and difficulty concentrating
Unlike IBD or infections, IBS rarely causes weight loss, fever, or blood in the stool, which should prompt medical evaluation. However, chronic discomfort and fatigue can affect mental health, leading to anxiety or depression, which in turn may worsen IBS symptoms.
Triggers of IBS
IBS symptoms are often triggered by a combination of dietary, psychological, and physiological factors. Identifying and managing these triggers is central to controlling the disorder.
Dietary Triggers
Certain foods are common IBS triggers, though sensitivities vary between individuals. Foods that can exacerbate symptoms include:
- High-fat or fried foods
- Processed foods with additives or artificial sweeteners
- Dairy in lactose-intolerant individuals
- Certain fruits and vegetables high in fermentable carbohydrates, also known as FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols)
- Caffeine and alcohol
Keeping a food diary can help identify personal triggers. Once identified, dietary adjustments can significantly reduce symptom frequency and severity.
Stress and Anxiety
Stress and anxiety have a profound impact on IBS. The gut-brain axis means that emotional stress can directly influence gut motility and sensitivity.
Chronic stress increases gut inflammation, alters hormone levels, and can disrupt the microbiome, contributing to bloating, diarrhea, or constipation. Individuals with anxiety or other mood disorders often experience more severe IBS symptoms. Addressing mental health through therapy, mindfulness, or relaxation techniques can reduce symptom frequency and improve quality of life.
Medications and Physiological Triggers
Some medications, including antibiotics, NSAIDs, and certain antidepressants, may trigger or worsen IBS symptoms. Hormonal fluctuations, infections, and previous gastrointestinal illnesses can also predispose individuals to IBS.
A subtype known as post-infectious IBS can occur after a gastrointestinal infection, even when the infection has resolved. Inflammation, altered gut motility, and changes in gut microbiota may persist, triggering ongoing IBS symptoms.
IBS and GERD
IBS often coexists with GERD (gastroesophageal reflux disease), with studies suggesting a significant overlap between the two conditions. While GERD primarily affects the esophagus, causing heartburn and acid reflux, IBS affects the lower gastrointestinal tract.
Shared risk factors include stress, dietary triggers, and abnormal motility of the gastrointestinal tract. Patients with both conditions may benefit from dietary strategies that address both acid reflux and bowel symptoms, stress reduction, and careful use of medications that affect the gut or stomach lining.
Diagnosis of IBS
IBS is diagnosed based on clinical symptoms and the exclusion of other conditions. There is no single test for IBS, making accurate diagnosis dependent on a thorough medical evaluation.
Key steps in diagnosis include:
- Detailed medical history, including symptom patterns and triggers
- Physical examination
- Blood tests to rule out anemia, thyroid disorders, celiac disease, or infections
- Stool tests to check for inflammation or infection
- The Rome IV criteria, which focus on recurrent abdominal pain associated with changes in stool frequency or consistency
Doctors may also recommend imaging studies or endoscopy if symptoms suggest other gastrointestinal conditions.
Dietary Management of IBS
Dietary modification is often the first-line approach for managing IBS. While triggers differ among individuals, several strategies are commonly recommended.
Low-FODMAP Diet
The low-FODMAP diet involves reducing foods that contain fermentable carbohydrates, which are poorly absorbed and can cause gas, bloating, and diarrhea. This diet is highly effective for many patients and should be followed under the guidance of a dietitian to ensure nutritional adequacy.
Fiber Management
Fiber has different effects depending on IBS subtype:
- IBS-C (constipation-predominant): Soluble fiber from oats, psyllium, or fruits can improve bowel regularity
- IBS-D (diarrhea-predominant): Insoluble fiber, such as wheat bran, may worsen diarrhea and should be limited
A gradual, personalized approach is recommended, as abrupt changes in fiber intake can trigger symptoms.
Hydration and Meal Patterns
Maintaining hydration is critical for bowel health. Small, frequent meals may reduce bloating and discomfort. Avoiding large meals, especially those high in fat, may prevent symptom flare-ups.
Probiotics
Some studies suggest that probiotics may help regulate gut microbiota and reduce bloating or discomfort. Effects vary depending on the strain, so professional guidance is recommended.
Medications for IBS
When lifestyle and dietary changes are insufficient, medications may be used to target specific symptoms:
- Antispasmodics: Reduce abdominal pain and cramping
- Laxatives or stool softeners: Used for IBS-C
- Antidiarrheal agents: Used for IBS-D
- Low-dose antidepressants: Help manage pain and symptoms linked to anxiety or stress
Medication choice is personalized based on symptom pattern, severity, and coexisting conditions. Regular follow-up is essential to monitor efficacy and side effects.
Lifestyle Approaches for IBS
Beyond diet and medication, lifestyle modifications can help reduce symptoms:
- Physical activity: Regular exercise supports healthy bowel motility and reduces stress
- Mindfulness and relaxation: Meditation, yoga, or deep-breathing exercises improve gut-brain communication
- Sleep hygiene: Adequate, consistent sleep enhances digestive health
- Avoiding smoking and excessive alcohol: Both can irritate the gastrointestinal tract and worsen symptoms
Managing IBS With Anxiety and Stress
Because IBS symptoms are often intensified by stress and anxiety, addressing mental health is key. Cognitive Behavioral Therapy (CBT) has shown significant benefits in reducing IBS symptom severity and improving quality of life.
Mindfulness-based stress reduction (MBSR) programs can help patients manage pain, bloating, and bowel irregularity, reinforcing the gut-brain connection in symptom control.
When to Seek Medical Attention
IBS is generally not life-threatening, but certain symptoms require prompt evaluation:
- Blood in stool or black, tarry stools
- Unexplained weight loss
- Persistent vomiting
- Severe or worsening abdominal pain
- Fever or other signs of infection
These symptoms may indicate more serious gastrointestinal conditions, such as inflammatory bowel disease or infections.
Frequently Asked Questions (FAQs)
- What is the difference between IBS and inflammatory bowel disease (IBD)?
IBS is a functional gastrointestinal disorder, meaning the intestines look normal but do not function properly. In contrast, inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis cause visible inflammation and damage to the intestinal lining. IBS does not increase the risk of cancer or cause permanent intestinal damage. - What are the most common triggers for IBS symptoms?
Common IBS triggers include certain foods (especially high-FODMAP foods), stress and anxiety, hormonal changes, gastrointestinal infections, and some medications. Triggers vary between individuals, which is why identifying personal patterns is essential for symptom control. - Can stress and anxiety really make IBS worse?
Yes. IBS is closely connected to the gut-brain axis, meaning emotional stress can directly affect bowel function. Stress and anxiety can increase gut sensitivity, alter motility, and worsen symptoms such as pain, bloating, diarrhea, or constipation. - Is the low-FODMAP diet safe and effective for IBS?
The low-FODMAP diet has been shown to reduce IBS symptoms in many people, particularly bloating, gas, and diarrhea. It is intended as a structured, short-term elimination diet followed by gradual food reintroduction and is best done under the guidance of a healthcare professional or dietitian. - When should someone with IBS see a doctor?
Medical evaluation is important if symptoms are severe, persistent, or worsening, or if warning signs such as blood in the stool, unexplained weight loss, fever, or persistent vomiting occur. These symptoms may indicate conditions other than IBS and require further testing.
Key Takeaways
Irritable Bowel Syndrome is a chronic functional disorder affecting the digestive tract, leading to abdominal pain, bloating, and changes in bowel habits. Symptoms are often triggered by dietary factors, stress, anxiety, medications, and coexisting conditions like GERD.
Effective management involves a combination of:
- Dietary strategies such as low-FODMAP diets and fiber management
- Medication guidance tailored to specific symptoms
- Stress reduction and mental health support
- Lifestyle adjustments, including exercise, hydration, and sleep hygiene
With early diagnosis, personalized treatment, and consistent management, individuals with IBS can achieve significant symptom relief and improved quality of life.